HemaShock® Physiology
Effects of HemaShock®
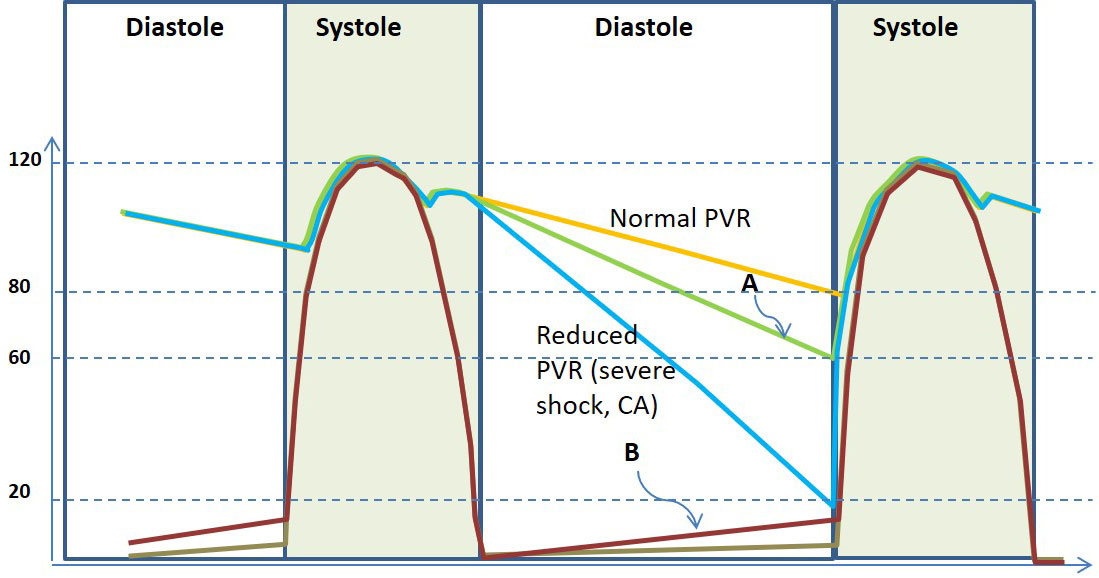
on Left Ventricular & Arterial Pressures
The circulatory effects of the application of HemaShock® can be summarized by using the typical cardiac cycle diagram shown above.
In this diagram, the pressure inside the left ventricle axis is seen (in brown or gray) to increase rapidly at the beginning of the Systole peak and then fall to near zero pressure. During the Diastole, the ventricular pressure increases gradually as the ventricle fills with blood.
The pressure in the aorta and the large arteries follows the ventricular pressure, once the aortic valve opens and the rapid ejection starts.
The aortic pressure continues to follow the ventricular pressure until the aortic valve closes. In normal circulation, the aortic pressure falls gradually, as more and more blood is supplied to the organs and tissues during the Diastole (orange line in the diagram). The rate of diastolic pressure fall is influenced by the resistance of the arteries and arterioles that lead to the organs and tissues. This resistance is called Systemic Vascular Resistance – SVR. The rate of diastolic pressure fall is also dependent on the cardiac output. If the cardiac output is low, or when the SVR is reduced, as may happen in shock or during CPR, the pressure during Diastole falls much faster than normal, as shown by the light blue line.
Changes in the Diagram When HemaShock® is Used
When HemaShock® is used it pushes blood from the limbs (legs usually) to the center. This blood increases the venous return to the heart so the filling of the left ventricle is improved, and the ventricular filling pressure incline during Diastole is steeper (brown line marked B). This increased ventricular filling increases the End-Diastolic Volume EDV of the ventricle, which, through the Frank-Starling mechanism, increases ventricular contractility, stroke volume, and cardiac output. However, HemaShock® has a second effect: it blocks the arterial flow into the limbs HemaShock® is placed on. This effect of HemaShock® impedes the flow out of the aorta to the limbs and has an immediate and direct effect on the SVR. Both effects (increased cardiac output and increased SVR) reduce the rate of fall of pressure in the aorta and main arteries during Diastole, as shown schematically in the green line marked A.
SUMMARY
The overall physiological effects of applying HemaShock® on a patient are:
- Increased Venous Return to the heart
- Increased Stroke Volume
Resulting in:
- Increased systolic blood pressure
- Increased diastolic blood pressure
Increasing diastolic blood pressure increases the coronary arteries perfusion since the blood supply to the cardiac muscle is predominantly during diastole.
The use of HemaShock® also reduces the ratio of unstressed to stress vascular volume.
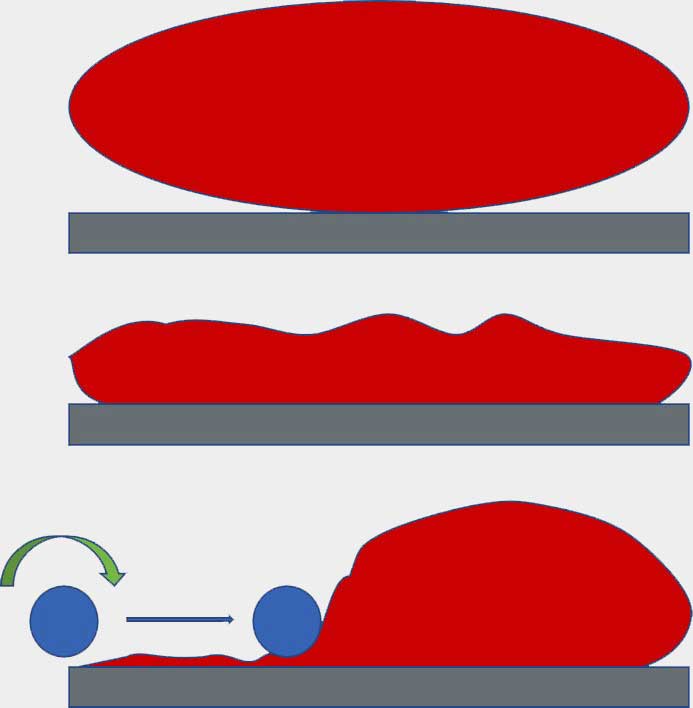
The Red Balloon Model of the HemaShock® Effect
on the Unstressed/Stressed Volume Ratio
When blood volume falls (e.g. due to hemorrhage or dehydration) or the volume of the blood vessels becomes pathologically large (e.g. due to sepsis, anaphylaxis, or drugs), the pressure in the system falls and the balloon “sags.”
Rolling HemaShock® (symbolized by the blue roller) over one part of the system (e.g. legs), and squeezing its content (blood) into the other part of the system (e.g. the central circulation), increases the pressure and stretches the latter. This, in fact, reduces the ratio of the unstressed to stressed volume in this part of the circulation.
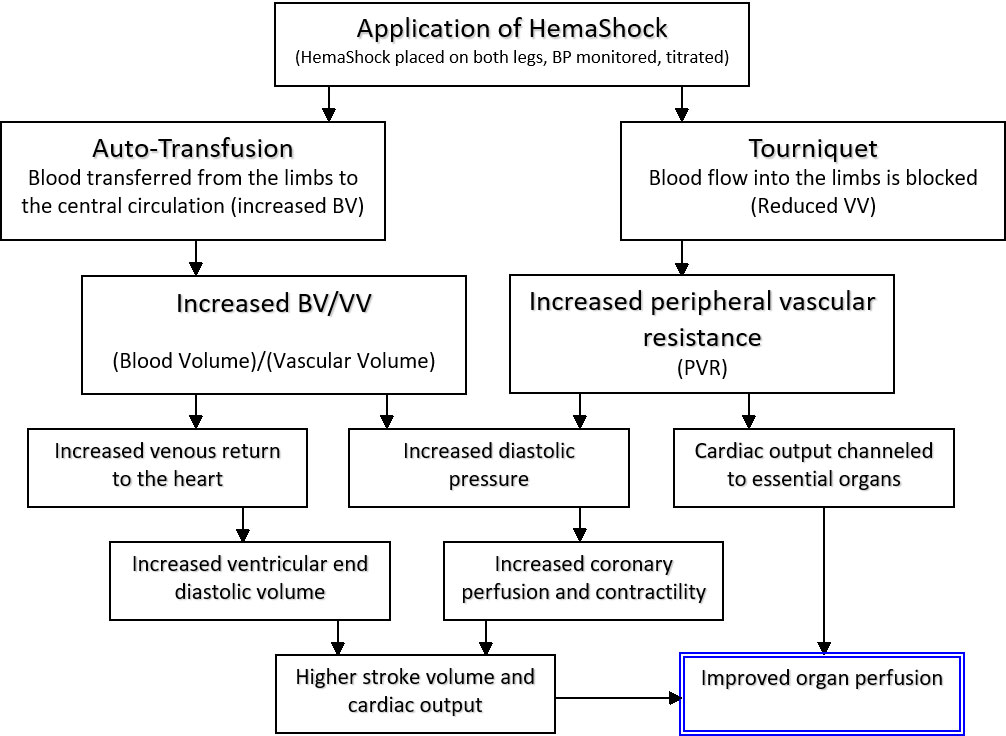
Physiological Effects of HemaShock® in Hemodynamic Shock
The rolling up of HemaShock® on a limb displaces blood to the central circulation. This is, in fact, a form of “Auto Transfusion” of the patient’s own blood (no risk of mismatch), in essentially the right temperature, with all of the needed clotting factors and oxygen carrying capacity (stored blood is anticoagulated, cold and depleted of 2,3, DPG, which shift the O2-Hemoglobin Dissociation Curve to the left thereby reducing its ability to transport oxygen to the tissues).
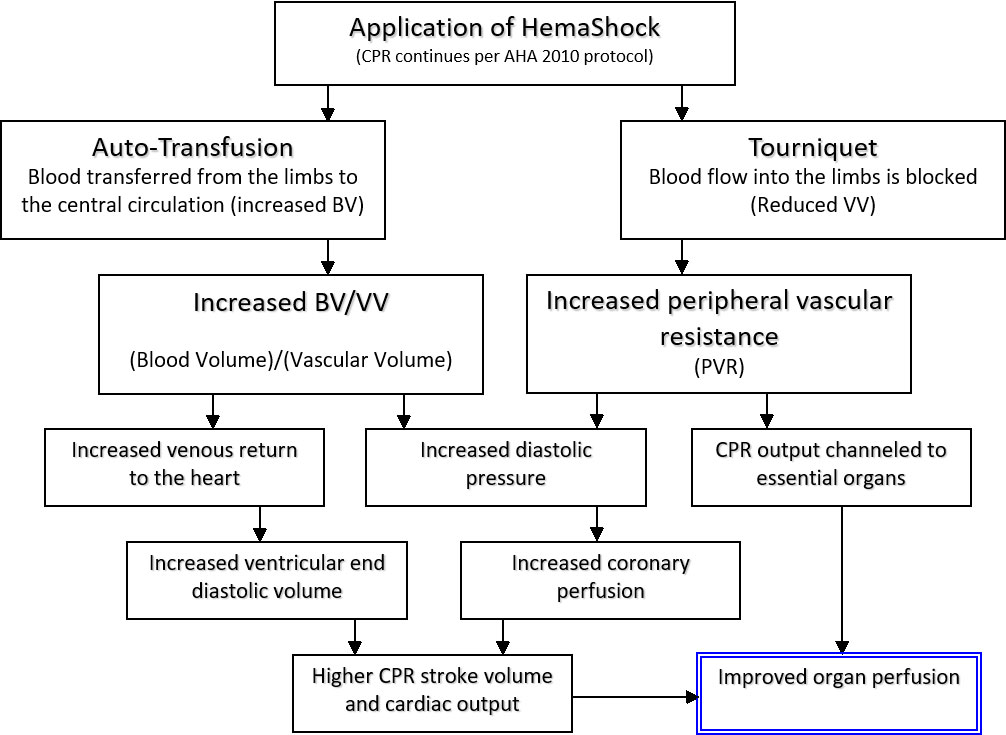
The autotransfusion effect increases the Blood Volume BV in the Central Circulation. The HemaShock® ring occludes arterial inflow into the limb, acting as a Tourniquet. By doing so, it increases the Peripheral/Systemic Vascular Resistance (PVR or SVR) and limits or reduces the Vascular Volume VV in which the patient’s Blood Volume resides. The ratio BV/VV in the central circulation is increased, venous return to the heart rises so that the ventricular filling and end diastolic volume EDV is higher, leading to a greater stroke volume and cardiac output. The higher diastolic pressure helps heart muscle perfusion via the coronary arteries, which further helps with cardiac performance.
Physiological Effects of HemaShock® during CPR in Circulatory (Cardiac) Arrest
Systolic blood pressure reaches 70-80 mm Hg and the diastolic pressure is not more than 20 mm Hg (see Hemodynamics During CPR – Bibliography). It is now accepted that the main reason for these low values is the very low venous return of blood to the heart.
This is caused by the loss of sympathetic tone that occurs almost as soon as blood flow to the brain is stopped. The blood vessels all around dilate and the blood pools in the periphery. (In fact, the main reason for using adrenalin and vasopressin during CPR is to counteract this extreme vasodilatation). Clearly, if blood is not returning to the heart, the chambers do not get filled, and as such, even if compressed very firmly, will not generate output. Bringing blood from the periphery to the heart is critical.
In recent years, a range of devices has been introduced to the emergency market with the intent to “suck” blood from the periphery to the chest. These include the Plunger method and its variants and the inspiratory threshold devices.
- It compresses the blood vessels in the limbs acting like a “mechanical vasoconstrictor” of sorts.
- It also blocks blood supply to the legs so that the generated cardiac output is channeled to the essential organs.
In addition, the increased PVR/SVR helps boost the diastolic blood pressure in the aorta which is key to effective coronary perfusion.
Hemodynamics During CPR – Bibliography
- Del Guercio LMR, Coomaraswany R, State D: Cardiac output and other hemodynamic variables during external massage in man. N Engl J Med 1963; 269: 1398.
- Jackson RE, Freeman SB: Hemodynamics of cardiac massage. Emerg Med Clin North Am 1983; 1: 501.
- Luce JM, Ross BK, O’Quinn, et al: Regional blood flow during cardiopulmonary resuscitation in dogs using simultaneous and nonsimultaneous compression and ventilation. Circulation 1983; 67: 258.
- Maier GW, Tyson GS, Olsen CO, et al: The physiology of external cardiac massage: High-impulse cardiopulmonary resuscitation. Circulation 1984; 70: 86.
- Paradis NA, Martin GB, Goetting MG, et al: Simultaneous aortic, jugular bulb, and right atrial pressures during cardiopulmonary resuscitation in humans: Insight into mechanisms. Circulation 1989; 80: 361.
- Ditchev RV, Winkler JV, Rhodes CA: Relative lack of coronary blood flow during closed chest resuscitation in dogs. Circulation 1982; 66: 297.
- Niemann J, Rosborough J, Ung S, et al: Coronary perfusion pressure during experimental cardiopulmonary resuscitation. Ann Emerg Med 1982; 11: 127.
- Sanders AB, Ogle M, Ewy GA: Coronary perfusion pressure during cardiopulmonary resuscitation. Am J Emerg Med 1985; 3: 11.
Physiological Validation of HemaShock®
Clinical Study on Healthy Subjects
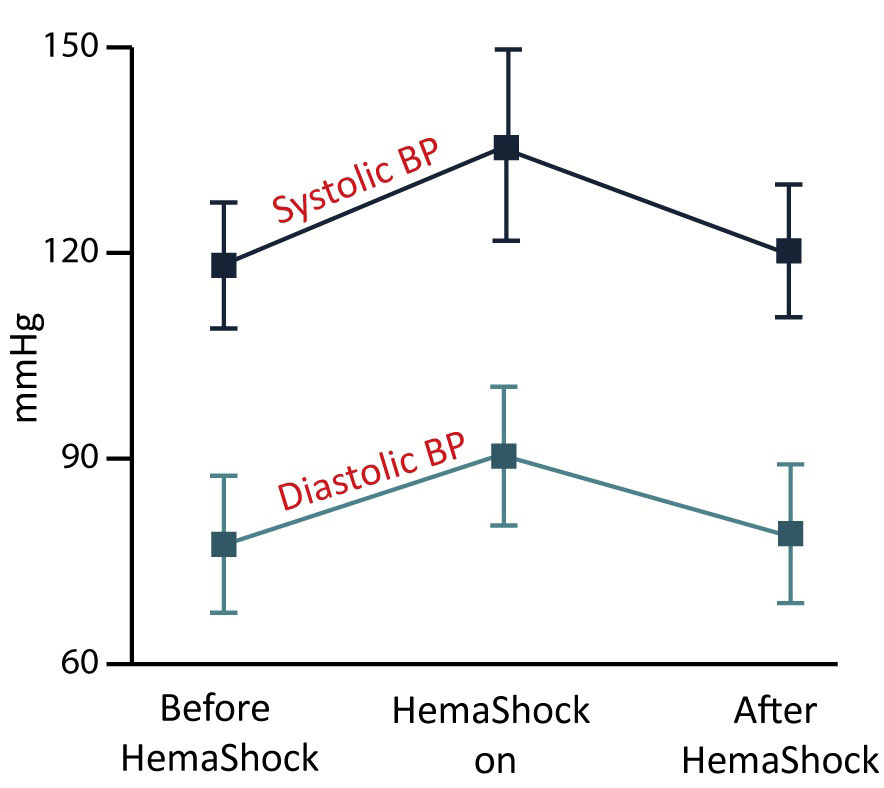
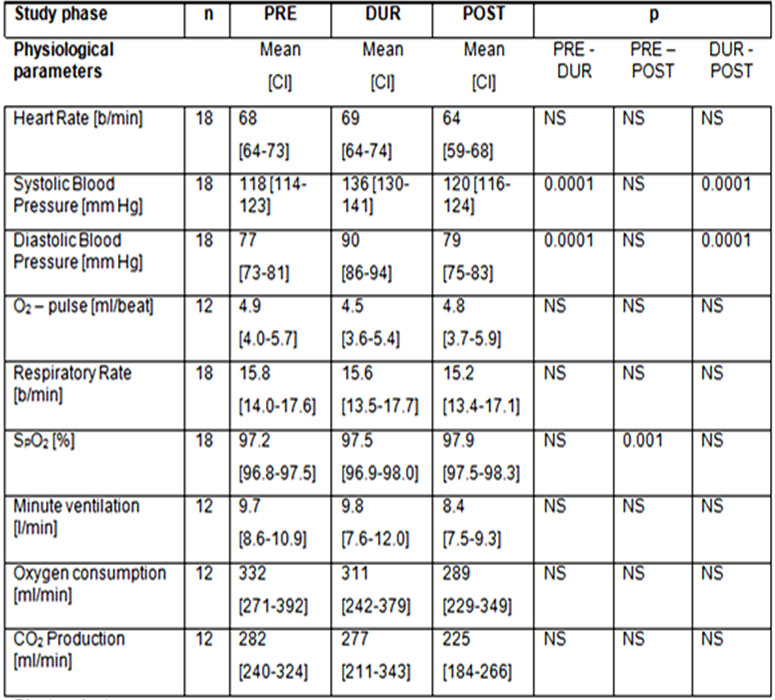
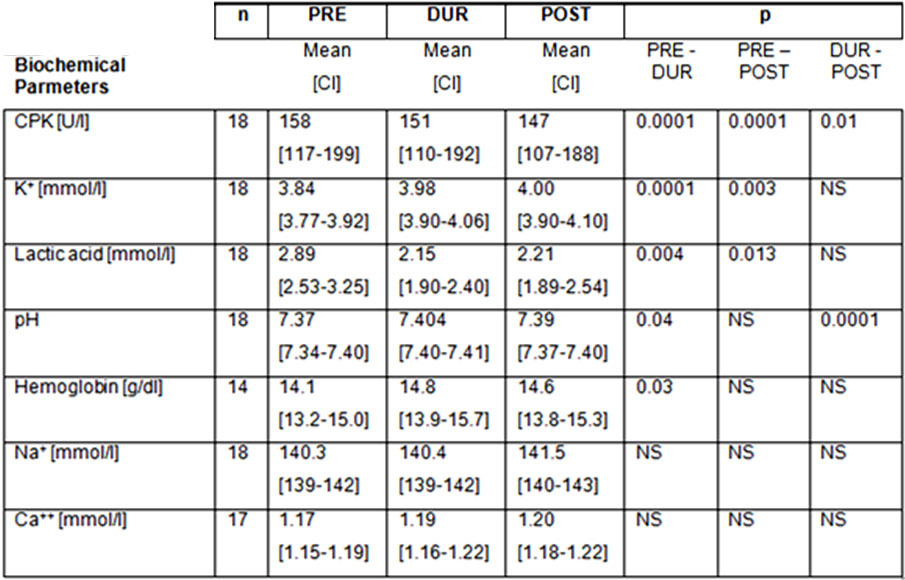
Feasibility, Usability, and POC – A Clinical Study. The physiological and biochemical effects of A-TT on 18 normal volunteers were assessed by applying the A-TT device on them for 20 minutes. It was observed that A-TT gave rise to 17.4; (14.5-20.3) (Mean; (CI)) and 13.1; (11.0-15.1) mm Hg rise in systolic and diastolic blood pressures, respectively (P < 0.0001)
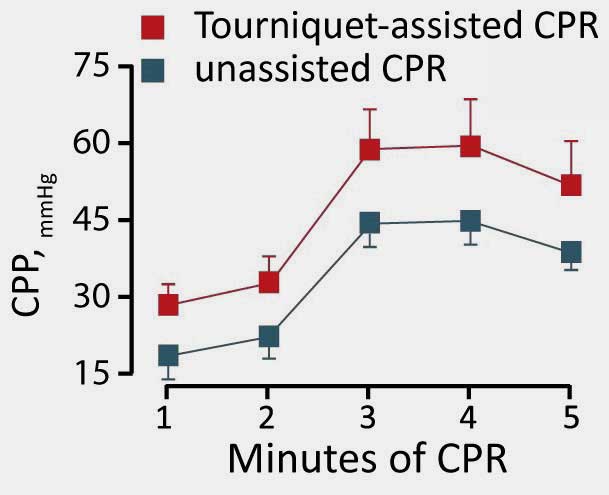
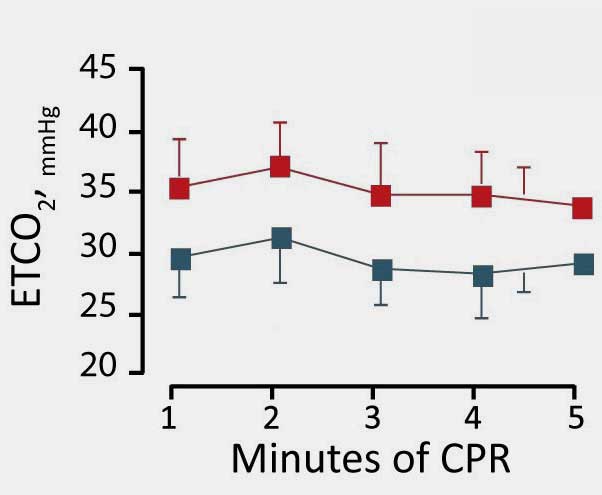
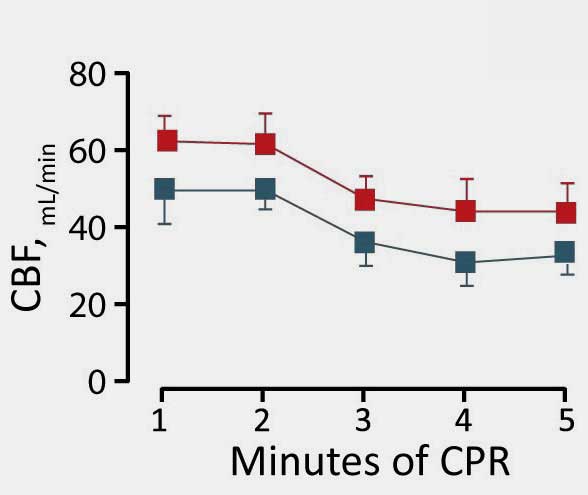
Animal Model: Tourniquet Assisted CPR
Thumper Cardiopulmonary Resuscitation was performed subsequent to inducing cardiac arrest in 10 animals; a control group of 5 underwent an unassisted CPR, while an Esmarch exsanguination tourniquet was placed on the limbs of 5 additional animals during resuscitation.
Results show that although no significant difference was found in defibrillation, doses of epinephrine or CPR duration in both groups, tourniquet-treated pigs presented significantly higher coronary perfusion pressure, End-tidal CO2 and cerebral blood flow.
These data demonstrate the effect of increased venous return and systemic vascular resistance on vital organ perfusion: the heart (CPP), the tissues (ETCO2) and the brain (CBF) all presently increased perfusion, just as expected with HemaShock®.